How to be Vigilant Against Breast Cancer [A Definitive Guide]
Self- examination pointers | Testing pointers | Defining high-risk category | Benefits of early detection | There is hope
On May 14, 2016, Amrita’s (name changed) life turned upside down. What was supposed to be a casual trip to merely accompany a close friend for her mammogram test at the polyclinic in Singapore turned out to be a painful eye-opener for Amrita. After her friend finished her check-up, the doctor casually asked Amrita to get hers done as well. So she did, not really expecting to find anything since she had been routinely examining herself.
The results sent her reeling with shock and disbelief. Apparently, the mammogram had detected a lump, deep behind her left/ right breast, cunningly hidden under layers of tissue and behind the aureole, which is why it kept evading detection during her self-examination routine. It could be malignant and could she get a biopsy done as well?
“I couldn’t believe what I was reading,” recalls Amrita. “This couldn’t be happening to me”. Her first thought was of her two kids and of all the things she had planned to do. Now, suddenly, without warning, there seemed to be a question mark on just how long she would live.
Finally, that same year, Amrita underwent a breast lumpectomy where a small amount of normal breast tissue around a potentially cancerous tumor was surgically removed. Hers was the size of a golf ball. The Bi-RADS (acronym for the Breast Imaging Reporting and Database System) score was 7. A score of above 3 usually gets recommended for a biopsy. So, Amrita underwent a biopsy as well.
The wait for the results was a nightmarish two weeks in which Amrita lost three kilos. The post-operative biopsy results were, thankfully, non-malignant. Ultimately, it wasn’t cancer but a fibroid that had sent confusing signals, although Amrita had veered very close to the edge.

“I just want women our age to know that all tumors don’t show up or can’t be felt when you are doing a self-examination. Don’ delay that mammogram, no matter how painful. Get it done,” is her appeal to all women her age.
So, if you are above 40, or pushing 50 or even more, here are the preventive steps that you can take because, remember: early detection can give you a fresh lease on life.
Self-examination pointers
Be regular in self-examination as it is important to catch any abnormal lumps or growths at the very initial stage itself.
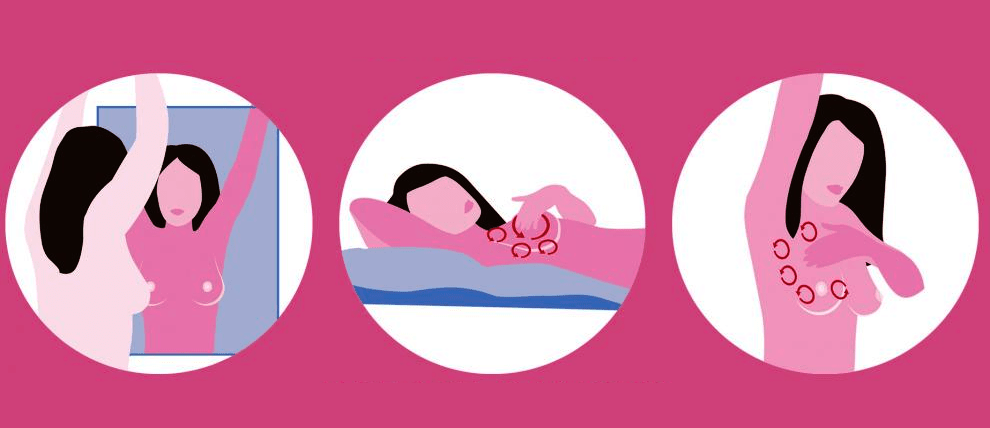
- Visual – Stand in front of the mirror to see whether both breasts are symmetrical. Is there any puckering? Has the size changed? Does the areola look any different? Any dimpling?
- Physical – Palpate your breasts from base, sides to the nipples to carefully feel for any lumps, any abnormal hardening within the tissue.
- Discharge – Squeeze from the base of the breast, around the areola to the tip of the nipple to see if there is any kind of discharge.
- Armpits – Check your armpits for any lumps or nodes. Breast cancer does not always develop in the breast; it can also grow in the nodes.
Testing pointers
There are different diagnostic tools that also indicate whether a lump is cancerous or not.
- 1.Chest X-Ray – A chest X-Ray can show up any initial abnormality and whether the cancer has spread near the lungs. Early detection via a chest X-Ray means that there is a much lower chance of the cancer metastasizing to other parts of the body if it is discovered while still restricted to one breast.
- Ultrasound– A new study by the Journal of National Cancer Institute shows that ultrasound can also be effective, less invasive and less expensive than a mammogram. Breast ultrasound can show certain breast changes, like fluid-filled cysts, that are harder to identify on mammograms.
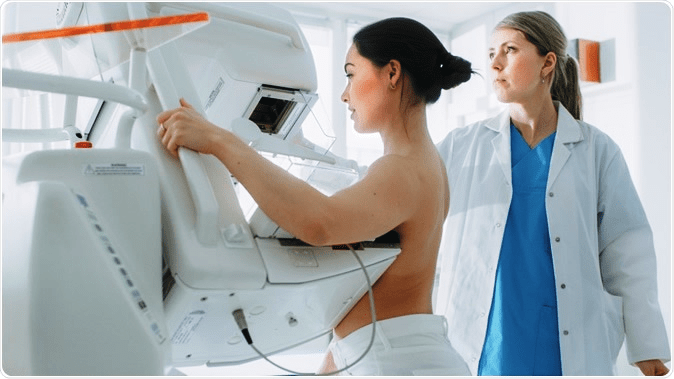
- Mammogram –A mammogram is an X-ray imaging test that examines breast health. It’s the most efficient tool to help detect breast cancer, especially at its earliest stage. And menopausal women, who are in the highest risk category, should absolutely have a mammogram done annually to eliminate the risks. A mammogram can often detect breast cancer even when it’s just starting out or even before a lump can be felt. At this stage the cancer is also the easiest to treat.
- Biopsy – It may sound scary, but a biopsy does not necessarily indicate you have breast cancer, only that your doctor wants to be doubly sure about it. If your other tests indicate that you might have breast cancer, your doctor will probably suggest a biopsy. The good news is that most biopsy results are not cancer, but a biopsy is the only way to be absolutely sure. During a biopsy, your doctor will surgically remove tiny pieces from the suspected area so they can be examined to see if they contain cancer cells.
So, who falls in the high risk category?
If you are a woman, you are already at risk! Having said that, there are certain groups that come under the high risk category.
- If you are a woman and are above 45 years. The chances of getting breast cancer increase with age. Most breast cancers are detected after 50 years of age.
- Genetic or hereditary mutations. You could have inherited some genetic mutations like BRCA1 and BRCA2 (BReast CAncer genes 1 and 2 that are the most well-known genes linked to breast cancer risk) that, unfortunately, increase the chances of getting ovarian or breast cancer.
- Reproductive history. Starting your periods before age 12 and entering menopause after 55 years increases the chances of getting breast cancer since a woman is exposed to a longer period of time to the estrogen hormone.
- Family history of breast or ovarian cancer. Your chances of getting breast cancer go up if your mother, aunt, sister or close family on either the mother’s or father’s side had a history of ovarian or breast cancer. Though this is not always the case, this does make you fall in the high-risk category.
- Menopausal women. After menopause, when the ovaries stop producing the hormone estrogen, it is the fat tissue in the woman’s body that becomes the main source of the hormone. Having more fat tissue means having higher estrogen levels, which can increase breast cancer risk.
Benefits of early detection
Not every lump is cancerous and not every cancer shows up as a lump. Some cancer cells are actually scattered like sand grains and only a mammogram can catch them. And early detection helps!
- Snaps you out of your complacency. Family history has nothing to do with it. 75% of women who get diagnosed with breast cancer have had no family history of the disease whatsoever. So, remaining in that false comfort zone could prove dangerous.
- Your chances of survival increase. Thanks to our unhealthy lifestyle and sedentary habits, cancer is on the rise. Mammograms catch breast cancer at its very early stage and help in increasing the chances of survival.
- As in Amrita’s case, a lump can’t always be felt. Let a more sophisticated equipment rather than your own hands or eyes be the best judge of what’s going on inside your breast.
There is hope!
Yes, the facts are grim. Yes, more women are diagnosed with breast cancer than any other type of cancer, besides skin cancer. Breast cancer is the most common form of cancer in India, having overtaken cervical cancer.
The survival rates of breast cancer in India are low because the detection takes place late. The only way to change these numbers is by increasing awareness. Breast cancer is a treatable disease and chances of survival are higher if it’s detected in time. The only way to do so is by being aware of how it can be detected and early diagnosis can be done.

In contrast, in the USA, according to cancer.net “Breast cancer is the second most common cause of death from cancer in women in the United States, after lung cancer. However, the number of women who have died of breast cancer in the USA has decreased by 40% from 1989 to 2007 thanks to early detection and treatment improvements.”
Food for thought
“These brushes with death, with the cancer threat looming large has changed the way I look at life now,” says Amrita, who is now absolutely fit and healthy and runs a successful counseling practice in Singapore. And only because a chance encounter led to something she had never ever imagined.
So, stop putting off that mammogram. Go for that test. Take your mother, sister, sister-in-law, or a female friend along. Anyone who falls in that age bracket. Prevention is always, always better than cure.
As women, let’s take ownership of this decision and rally other women to come along and beat this beast to pulp!

![How to be Vigilant Against Breast Cancer [A Definitive Guide] How to be Vigilant Against Breast Cancer [A Definitive Guide]](https://www.dayamukherjee.com/wp-content/uploads/2020/10/breast-cancer-awareness.png)
No Comment